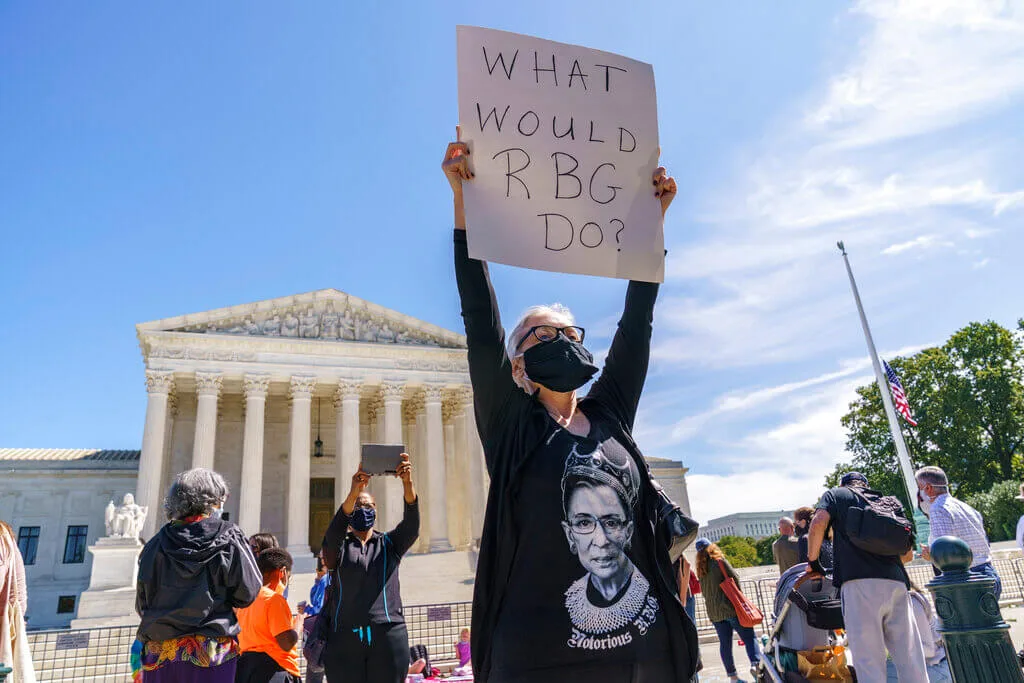
Kelli Midgley, center, an English teacher from Baltimore, joins people gathered at the Supreme Court to honor the late Justice Ruth Bader Ginsburg, in Washington, Saturday, Sept. 19, 2020. Ginsburg's death leaves a vacancy that could be filled by a more conservative justice by President Donald Trump. (AP Photo/J. Scott Applewhite)
The healthcare law is in front of the Supreme Court once again in November, so COURIER decided to answer some of the most frequently asked questions about the ACA.
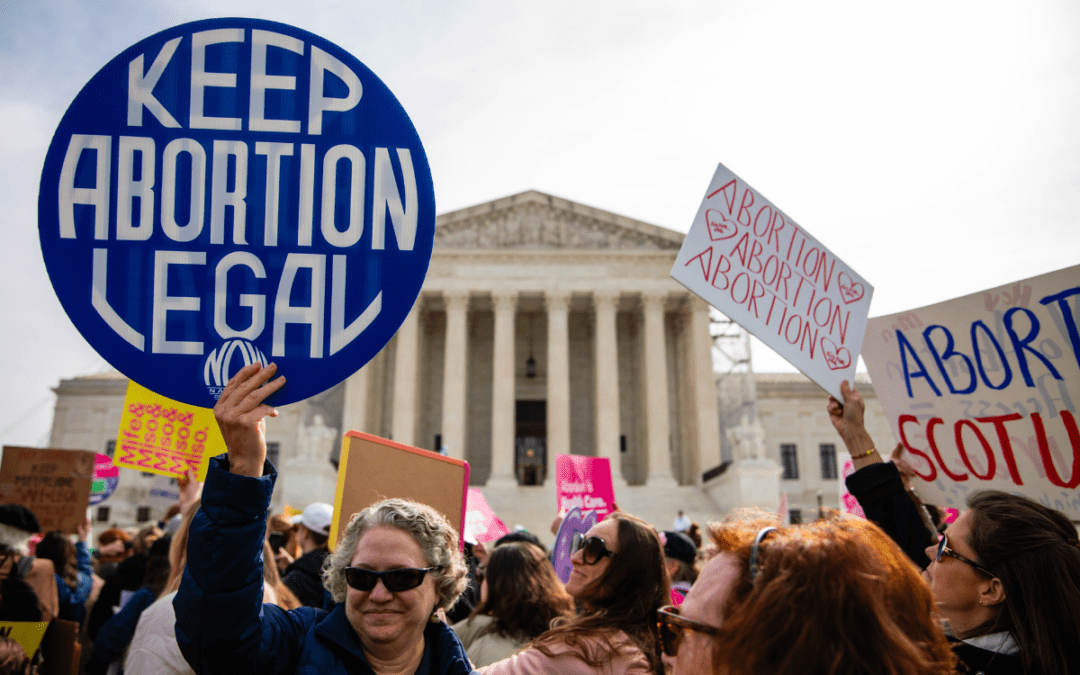
The death of Supreme Court Justice Ruth Bader Ginsburg on Friday and the potential appointment of a new, conservative judge could endanger health insurance coverage for more than 20 million people and critical protections for tens of millions more who live with pre-existing medical conditions. The conservative-leaning court is set to hear a case on November 10—one week after the general election—in which 18 Republican-led states, with the backing of President Donald Trump, are suing to repeal the Affordable Care Act (ACA).
While the ACA was initially unpopular, the law now receives broad public support and has become a critical lifeline for many Americans. Several Republican politicians now claim they support guaranteeing protections for people who live with pre-existing conditions, such as diabetes, cancer, and heart disease. But some of the same candidates, including Colorado Sen. Cory Gardner, previously voted to repeal the ACA, which guaranteed these very protections for the first time.
With the future of Ginsberg’s seat up in the air and ACA facing perhaps its greatest threat yet, COURIER decided to answer some of the most frequently asked questions about the law.
How does the Affordable Care Act protect people with preexisting conditions?
Before the ACA was passed, people with health conditions were often denied coverage outright, offered minimal coverage, or forced to pay for extremely expensive plans. Under the law, however, it is illegal for health insurance companies to deny coverage to people with pre-existing conditions or charge them higher rates for coverage.
What does the Affordable Care Act do?
The law dramatically expanded access to both public and private health insurance, increased protections for patients, established programs to prevent illness, banned insurers from implementing financial limits on coverage, and mandated insurers cover pre-existing conditions and certain essential benefits, such as prescription drugs and mental health and substance use disorder services.
Is the Affordable Care Act still in place?
Yes. The ACA remains in place, despite the best efforts of Republicans, who have tried to repeal the law dozens of times. But the landmark healthcare program is hanging on by a thread and faces yet another existential threat with the upcoming Supreme Court Case in November.
When was the Affordable Care Act passed? When did it start?
The federal government passed the ACA in March of 2010 and the law’s measures began being phased in soon after, though the ACA’s key benefits were not fully implemented until 2014.
How many Americans get health insurance from the Affordable Care Act?
More than 23 million Americans now rely on the ACA for insurance coverage, according to recent estimates from the Center for American Progress.
Who qualifies for the Affordable Care Act?
Anyone who does not receive health care insurance through their job or a public insurance program, such as Medicare or Medicaid, can purchase health insurance on the ACA’s health insurance marketplace or affiliated state-level marketplaces.
The law also incentivized states to expand access to Medicaid, allowing millions more low-income adults to obtain insurance coverage through the program. Thirty-six states and Washington D.C. have expanded Medicaid and three more are in the process of doing so. Residents living in states that opted to expand their programs can determine their eligibility for Medicaid here.
What is maximum income or minimum income to get the Affordable Care Act in 2020?
There is no maximum or minimum income to purchase coverage on the ACA’s marketplace, but many people may be eligible for cost-sharing programs to reduce out-of-pocket costs and federal tax credits to reduce premiums. This assistance depends on income level and household size. You can begin to determine your eligibility for tax credits or cost-sharing programs here.
There is, however, a maximum income to qualify for the ACA’s Medicaid expansion. This cap varies by state, but in most states, applicants must earn below 138% of the federal poverty line (FPL) to qualify for Medicaid based on income alone. The 2020 FPL income numbers are:
- $12,760 for individuals
- $17,240 for a family of 2
- $21,720 for a family of 3
- $26,200 for a family of 4
- $30,680 for a family of 5
- $35,160 for a family of 6
- $39,640 for a family of 7
- $44,120 for a family of 8
How do you calculate income for the Affordable Care Act?
Income does not impact eligibility for coverage, but as we mentioned earlier, it can affect what financial assistance you might be eligible for. You can use this income calculator to determine what savings you may be eligible for under the ACA.
When is open enrollment for the Affordable Care Act?
The Open Enrollment Period to purchase coverage for 2021 through the ACA Marketplace runs from Sunday, Nov. 1 to Tuesday, Dec. 15, 2020. Some states with their own marketplaces have longer enrollment windows. The states with their own insurance exchanges are: California; Colorado; Connecticut; the District of Columbia; Idaho; Maryland; Massachusetts; Minnesota; Nevada; New Jersey; New York; Pennsylvania; Rhode Island; Vermont; and Washington.
Residents of those states can find more information about their enrollment period here.
Many people may be eligible to obtain coverage prior to the open enrollment period, however, if they meet one of the criteria, which include loss of private insurance coverage, change in household size, and change in income.
Does the Affordable Care Act cover a colonoscopy?
Yes. Under the ACA, most private insurance plans must provide a no-cost series of preventive services, including vaccines and screening tests such as colonoscopies, diabetes tests, lung cancer screenings, HIV screenings, services for pregnant women, and various tests for children. Insurance companies may not impose copayments or other out-of-pocket costs on patients for receiving these services.
The only exception to the rule are those insurance plans that were “grandfathered” in prior to March 23, 2010 and do not make substantial changes to their coverage, such as increasing patient cost-sharing or cutting benefits.
Politics
How Project 2025 aims to ban abortion in Pennsylvania
Former president Donald Trump said abortion was a state’s rights issue recently, but conservative organizations, under the banner “Project 2025,”...

736,000 PA households could lose crucial help on their internet bills
Time is running out for the Affordable Connectivity Program, which provides low-cost high speed internet access for over 736,000 Pennsylvania...

What to know about Trump’s legal issues
Over the past year, former president Donald Trump has become the center of not one, not two, not three, but four criminal investigations, at both...
Local News

Conjoined twins from Berks County die at age 62
Conjoined twins Lori and George Schappell, who pursued separate careers, interests and relationships during lives that defied medical expectations,...

Railroad agrees to $600 million settlement for fiery Ohio derailment, residents fear it’s not enough
Norfolk Southern has agreed to pay $600 million in a class-action lawsuit settlement for a fiery train derailment in February 2023 in eastern Ohio,...






