Bucktail Medical Center in Clinton County is struggling financially and has launched a GoFundMe campaign to keep its doors open for the immediate future.
When you say Pennsylvania, most people think of Philadelphia and Pittsburgh, two large cities in the state with a variety of options for housing, employment, and health care.
But for the more than 3 million Pennsylvanians who live in one of the 48 rural counties in the state, life is a little bit different.
There’s a sense of community that bonds people who live in less populated areas of the state. Those in rural communities are also faced with significantly limited options for essential services like medical care and transportation compared to those who live in and around Pennsylvania’s largest cities.
For residents of the small town of Renovo, those options for health care are in danger of becoming even more limited. The western Clinton County town — population just over 1,000 — is facing the potential loss of its only medical clinic, Bucktail Medical Center, due to financial issues. Bucktail CEO, Tim Reeves, is hoping that sense of community will help pull the medical center through this financial rough patch and allow it to remain open.
Reeves has started a GoFundMe campaign for the medical center, hoping to raise $1.5 million to give the facility some breathing room so they can implement new programs in the hopes of bringing in more revenue and thus making the facility financially viable.
“I’m concerned about meeting the next payroll,” Reeves said. “I’m concerned that the people living in western Clinton County will lose not only medical care close to home, but also their largest employer.”
Bucktail is a community-owned healthcare facility with a 16-bed critical access hospital, a 43-bed nursing facility, 24/7 emergency room, a community clinic, and an ambulance service. It is the only provider of medical and ambulance services in the area. And, like other hospitals in rural areas, it is facing a financial crisis.
According to a recent report by the Center for Healthcare Quality and Payment Reform (CHQPR), rural hospitals are closing at an alarming rate across the country. From 2010 to 2021, 136 rural healthcare facilities closed. Nineteen of those occurred in 2020 alone, a record for hospital closures.
“Small rural hospitals are being forced to close because they are not paid enough to cover the cost of delivering care to patients in rural areas,” the CHQPR report said. “Most small rural hospitals lose money delivering services to patients, while most urban hospitals and larger rural hospitals make profits on patient services.”
Lisa Davis, director of the Pennsylvania Office of Rural Health, said there are now eight counties in the commonwealth that do not have a hospital. The most recent closure of a rural hospital in the state was in Wyoming Valley, Wyoming County, last year. Wyoming County has a population of almost 27,000 people over an area of 401 square miles. That’s a large area to be without a hospital, Davis said.
“This is an especially critical time for rural hospitals in Pennsylvania,” Davis said. “Services have become much more expensive to offer. The way care is delivered has evolved. Things aren’t the same as they were decades ago and rural areas are really shouldering the brunt of it. It’s a real detriment to the community overall to lose healthcare services.”
Other rural healthcare facilities have been forced to close certain departments, such as Labor and Delivery, due to financial issues and low patient volumes, Davis said. So while some rural counties still maintain a hospital or healthcare facilities, services may be limited which could mean forcing women in labor to drive further away to get the care they deserve when delivering their babies.
Financial struggles
According to the CHQPR report, small rural hospitals lose money on patient services because of inadequate payments from private insurance plans, whereas urban hospitals and larger rural hospitals make large profits on services to patients with private insurance. The majority of patients in a rural hospital like Bucktail rely on Medicare or medical assistance, whereas urban hospitals see larger volumes of patients with private insurance.
Exacerbating the issue of low reimbursement rates, Reeves said, is low patient volumes.
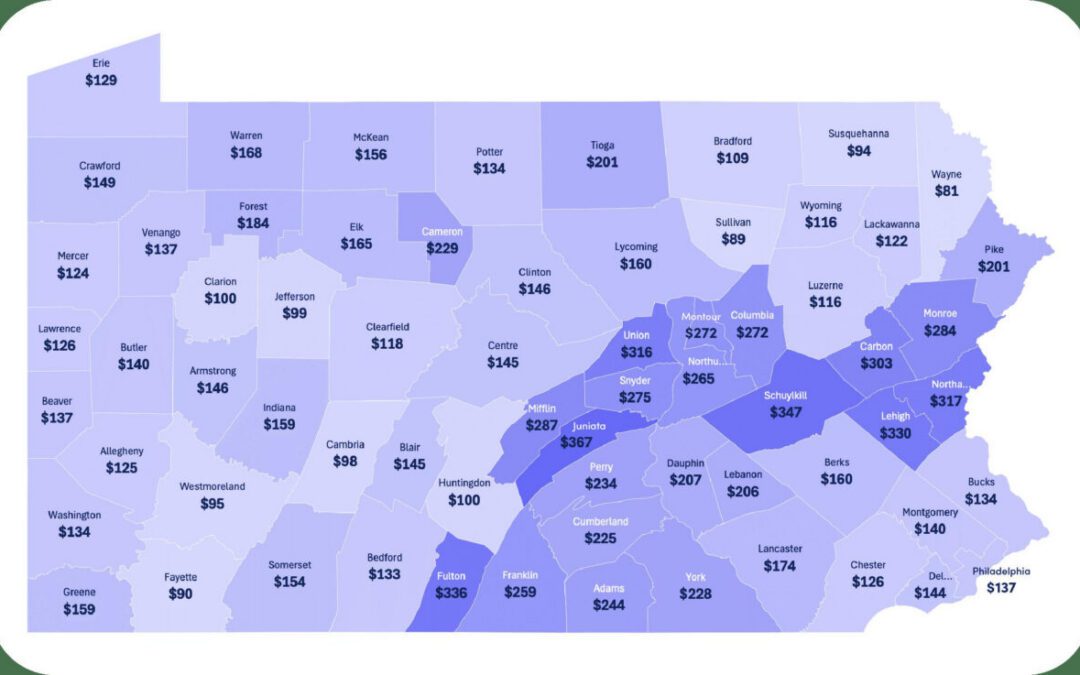
Standard payments for hospital services are not large enough to cover the higher cost of delivering services in small rural communities. The average cost of an emergency room visit, inpatient stay, laboratory test, imaging study, and primary care visit is inherently higher in small rural hospitals and clinics than at larger hospitals. That’s because there is a minimum level of staffing and equipment required to deliver each of these services regardless of how many patients a hospital treats on a daily basis.
“I need to have a doctor in my ER 24 hours a day 7 days a week,” Reeves said. “It doesn’t matter if we see zero patients or 100 patients, a doctor has to be there. Plus I have the cost for nurses, and I still need to clean up and buy supplies.

Tim Reeves, CEO of Bucktail Medical Center
“What that boils down to is my cost per patient is significantly higher than a hospital like CHOP’s (Children’s Hospital of Philadelphia) cost per patient. They aren’t losing money by having a doctor in their ER every day because they have the patient volume to support it. We don’t have that patient volume.”
While Bucktail does not receive funding from the state government, there are ways for the legislature to help. Over the years, bills amending how healthcare facilities are reimbursed through Medicaid and other insurance companies, as well as their reimbursement bargaining power with insurers have been introduced, yet passage of those bills has been thwarted by Republicans.
The consequences of closure
Davis said, oftentimes, the largest employers in a rural area are the local hospital.
“The hospital is usually one of the top three employers in a rural community,” Davis said. “When a rural hospital closes it really knocks down the morale of a community. It sends the message that you aren’t worthy of care. And it really impacts economic development because employers may not want to stay, expand, or relocate to a place where there is no healthcare services.”
Bucktail has 85 employees and is the biggest employer in the western part of Clinton County.
If Bucktail is forced to close, that’s 85 people who will lose their jobs which, in turn, will hurt the local economy.
“Every dollar that is spent in a rural community is estimated to roll over one-and-a-half times as it is reinvested in that community,” Davis said. “The only way economic development and jobs can be created in rural communities is if there is a viable healthcare system in the community.”
Another, more alarming consequence of a potential Bucktail closure, is the potential loss of lives.
The center services an area of 3,100 people. According to Reeves, the next closest emergency room is in Lock Haven which is 28 miles away, a 37-minute drive down a two-lane country road. That facility closed all inpatient and surgical services in April of this year.
The next closest hospital with inpatient services is Geisinger Jersey Shore which is 40 miles away, a 50-minute drive down the same two-lane country road.
If the medical center closes, there would be no healthcare services available in the area. No ER, no blood tests, no X-rays, no medical appointments, no nursing home, and no ambulance.
“The community we serve is about 3,100 people,” Reeves said. “Not a really large area, but the question becomes ‘Do they still deserve to have the same basic healthcare as everybody else in the US?’ If the answer is yes, we have to find a different way to fund that. If the answer is no, then we are saying that, as a country, we are willing to accept disproportionate healthcare based on where you choose to live.”
Since Bucktail has the only ambulance service in the area, its closure means the next closest ambulance for Renovo residents would be almost 30 miles away, a 35-minute drive one way. And with 85% of the patients that come in on medical assistance or Medicare, according to Reeves, lack of transportation becomes a legitimate barrier to accessing health care.
“An hour trip from here to Williamsport and back is half a tank of gas for you and me,” Reeves said “For these people, it’s sometimes an insurmountable goal. They don’t have the resources.”
Long-term solutions
While the GoFundMe campaign — which started at the end of August and has raised $15,880 so far — would help Bucktail if it’s successful, Reeves said other issues need to be addressed to ensure long-term viability.
“We’ve created a master plan and have come up with some potential programs and projections that give us the potential to thrive,” Reeves said. “But we need to get from here to there.”
The center has secured a US Department of Agriculture Emergency Rural Healthcare grant to replace a leaking roof, update the antiquated heating boilers, replace leaking water pipes, and purchase necessary equipment. And the center’s first ever CT scanner is set to arrive by the end of the month.
Reeve said the center plans to reduce costs by directly hiring physicians and eliminating costly agency staff. He is also working to negotiate contracts with insurance companies in the hopes of getting higher reimbursement rates.
“We’ve spent a lot of time evaluating what our community needs and what we can change to meet those needs,” Reeves said.
But above all, what would help Bucktail the most is an increase in patient volumes, Reeves said, acknowledging the unusual nature of a hospital seeming like it’s trying to drum up business.
“If we are going to survive, patient volumes are going to have to increase,” Reeves said. “Yes, you can get your blood work done elsewhere but you also do have the choice to have it done here. You can do it here and support your local hospital. Come to our ER rather than traveling down the road. I can guarantee you’ll see a doctor faster. Our staff is great at dealing with anything.
“We don’t want more people to get injured or sick, we just want more injured or sick people to come here.”
During a recent public meeting to make the community aware of Bucktail’s financial situation, Reeves said the following to attendees:
“This is your community, your hospital, your choice. You guys own this. It’s yours. It’s not mine. It’s not the board of directors. It belongs to the community. If you want it here, the best thing you can do is make sure you use it. If you aren’t willing to do that, there is only so much the rest of us can do. There are only so many rabbits you can pull out of the hat. At some point your options dry up.”
While the situation looks dire for Bucktail, Reeves said that he has been buoyed by the kindness of others, and still believes that he and his staff are here for a reason, and need to keep fighting hard to keep the doors open.
The municipal water authority is forgoing Bucktail’s payment for the next two quarters. That’s a savings of around $5,000, Reeves said. The municipal sewer authority also waived a quarter of its charges for the center.
A local company donated two tires for Bucktail’s’s ambulance. And another company has offered to do the Bucktail’s billing and collections free for 90 days.
“We keep seeing these small miracles,” Reeves said. “Every week there is something that really shouldn’t happen but it does. Every week somehow I’ve been able to make payroll. I don’t know how long that continues but we have to be encouraged when we see these little things. You have to believe that there is a reason why it happens. I have to believe that happens because we need to be here.”
Davis agrees. And also credits it to the rural way of life, and its inherent togetherness that you just can’t find in the cities.
“Small rural hospitals are absolutely committed to providing high quality healthcare services to their community,” Davis said. “The reason they work so hard to stay open is because they want to provide these services. They want to stay open — they don’t want to tell their community they aren’t worthy of services. That’s the great part of rural areas. Everyone is worthy and they all work together to make sure life is good for each other.”
Support Our Cause
Thank you for taking the time to read our work. Before you go, we hope you'll consider supporting our values-driven journalism, which has always strived to make clear what's really at stake for Pennsylvanians and our future.
Since day one, our goal here at The Keystone has always been to empower people across the commonwealth with fact-based news and information. We believe that when people are armed with knowledge about what's happening in their local, state, and federal governments—including who is working on their behalf and who is actively trying to block efforts aimed at improving the daily lives of Pennsylvania families—they will be inspired to become civically engaged.
One in 5 ACA enrollees in Pa. drops health coverage as costs spike
About 85,000 Pennsylvanians have dropped their Affordable Care Act coverage for 2026 in the face of soaring premium costs from the expiration of...

It’s 2026 and you’re uninsured. Now what?
It’s 2026, and you’re uninsured. Now what? Renuka Rayasam February 2, 2026 Health policy changes in Washington will ripple through the...

Two community hospitals in York County set to open this spring
Two new community hospitals in York County are expected to open in the spring, according to WellSpan's advertisements. One of the hospitals is just...

Report: Pa. hospitals face increasingly precarious financial future
Financial instability could force closures at more than a dozen Pennsylvania hospitals in the coming five years if state policymakers fail to act...

Pa. Pennie enrollment drops as Congress wrestles with health insurance subsidy vote
Some Pennsylvanians stay enrolled and pay tripled premiums with the hope lawmakers will vote to extend tax credits. Thousands of Pennsylvanians have...